About Ankle instability
Ankle instability typically occurs after the ligaments in the ankle have stretched out, losing the normal stability of the bones in the ankle and foot. This can be a result of an injury or occur over a long period of time from poor foot positioning, bad shoe wear or genetic predisposition.
When there is ankle instability the probability of further ankle sprains increases significantly. While the ligaments themselves may not be able to shorten back to normal, the muscles supporting the ankle can be strengthened to take up the slack. This compensation allows for better stability in the ankle and foot with walking, running and sports. Bracing may also be needed depending on the severity of the instability.
How physical therapy helps
Our physical therapists work with different physicians, including podiatrists to rehabilitate ankle and foot injuries. By assessing your ankle and foot joint movements we can determine what areas need to be strengthened bringing support and stability to your ankle.
With years of training in analyzing and treating joint mechanics, walking and movement, we put together a custom treatment plan that will improve your ankle stability. Call us today to discover how we can help increase your ankle stability!
Ankle Sprain / Strain
Ankle sprains are very common injuries and typically occur from improper footwear on uneven terrain. Most often, sprains occur from sports or trips over objects that were unseen. Sprains refer to injuries of the ligaments (connect bone to bone) and strains refer to injuries of the muscles or tendons (connect muscle to bone). Sprains and strains occur from quick over-stretching of the tissues causing micro-tearing and subsequent injury. Swelling begins as part of the inflammation process, causing pain and difficulty with movement.
The first step in treating sprains or strains in the ankle is to rest, ice and elevate it. Common sprains in the ankle occur on the outside of the ankle where 3 main ligaments attach. There are different levels of sprain or strain from mild to severe. With severe limitations in movement you should see your physical therapist right away. In some cases, the tearing can be complete and even be in need of surgical repair.
How physical therapy helps
In most cases, physical therapy can effectively help you recover from a sprain or strain. We first evaluate the injured area to determine the extent of the injury and ensure that the ligaments or tendons are still intact. We then formulate a treatment plan that will quickly relieve your swelling, pain and begin restoring range of motion.
The goal of physical therapy is to restore your normal range of motion and eventually restore normal strength. If you participate in sports or are very active, we will work closely with you to make sure that you fully recover and can participate in those activities you love to do. Call us today to discover how we can effectively treat your ankle sprain or strain.
Information coming soon!
What is Sciatica?
Sciatica is the term used to describe radiating pain into the buttock that can travel down the back of the thigh. Often this pain is achy and spread out along these areas. Sciatica is a result of irritation to the sciatic nerve, which travels deep in the buttock and down the back of the leg. In about 20% of people, the sciatic nerve pierces through the piriformis muscle deep in the buttock instead of under it. This can make the sciatic nerve more susceptible to irritation and pressure from the piriformis muscle. The piriformis muscle helps guide hip movement, but can become very tight with prolonged sitting. This increased tightness causes pressure and irritation to the sciatic nerve causing pain.
What is Radiating Pain?
Radiating pain to the leg doesn’t necessarily mean you have sciatica, but it does tell you that something is wrong. Irritated muscles and tissue often can radiate pain. Spread-out, achy pain is often indicative of this type of problem. Sharp, stabbing pain with numbness or tingling is more nerve irritation or compression occurring in the low back or leg. These types of sensations typically occur to specific parts of the leg.
How physical therapy helps
Physical therapy is one of the best treatments for Sciatica and radiating pain into the leg. It first takes a thorough evaluation to determine where your problem is starting. Our physical therapists take time to examine the movement of your spine, hips and legs. Range of motion, strength, joint mobility and muscle condition are assessed by our physical therapists. After we determine the root cause of your problem, we put together a comprehensive plan to quickly relieve your pain, relieve your radiating symptoms, improve your range of motion, improve strength and help you to prevent future episodes.
With gentle, specialized hands-on techniques we work to improve your spinal and hip mobility, reducing pressure on your sciatic nerve. In addition, modalities such as heat, ice, electrical stimulation and ultrasound may be used to reduce inflammation and resolve your pain quickly. We then perform gentle stretching and strengthening exercises to restore your normal motion and strength. This results in lasting effects that will stop your pain from returning. Call us today to find out how we can relieve your Sciatica and radiating leg pain, returning you to the activities you love.
Information coming soon!
Information coming soon!
As is often the case with many diagnoses ending in “Syndrome,” Restless Legs Syndrome (RLS) can be elusive and challenging to diagnose, treat, and understand. While we sometimes work with patients who come to us primarily for help with RLS (yes, we do treat it), more often they are seeking treatment for some other problem and happen to mention they have RLS. In an effort to promote understanding of this condition, we have compiled this summary from the limited literature on RLS as well as our clinical experience.
What is RLS?
RLS is generally characterized by an urge to move and the feeling of unpleasant sensations inside the lower legs.1 Generally symptoms will affect both lower legs. Symptoms of RLS usually occur during periods of inactivity and resolve with movement or exercise. Typically at night time when attempting to rest is when symptoms are the worst, but problems can also be present during the day.
How is it Diagnosed?
As with many “syndromes,” there are no tests that absolutely confirm RLS. It is a diagnosis based purely on symptomology and the absence of other diagnoses that would account for the symptoms. The International Restless Legs Syndrome Study Group established criteria for diagnosis which include: a desire to move the limbs, usually associated with paraesthesia (pins and needles sensation) or dysaesthesia (abnormal sensation); motor restlessness; symptoms worse or exclusively present at rest; symptoms worse in the evening or night.2,3 Additional features that may accompany these signs or symptoms include: sleep disturbance, periodic limb movements in sleep, a normal neurological examination, chronic symptoms with exacerbations and remissions, and a positive family history.2 The establishment of such criteria indicate there are enough people with these complaints to justify studying them. However, establishing these criteria does not provide an explanation as to the cause or provide guidelines for treatment.
Why does it occur?
There are several unproven hypotheses attempting to explain RLS. The most common one cites iron deficiency, which can be identified with basic blood testing. But consider this: many people with iron deficiency do not have RLS, and many people with RLS do not exhibit iron deficiency. Then there are those with iron deficiency who still suffer with RLS even after their iron levels have been normalized. Certainly, normalizing iron levels in the body is desirable for many reasons. But logic dictates that this does not fully explain or address the problem for many individuals. If iron deficiency was the cause and the solution supplementation, then there would be no market for pharmaceuticals specifically targeting RLS. Yet the two most frequently prescribed medications, Pramipexole (Mirapex) and Ropinirole (Requip), are in high demand. Another proposed cause of RLS is dysfunction of dopamine (a neuro-transmitter affecting movement), although this also is unproven.
There is a growing body of literature and evidence supporting the phenomenon of myofascial trigger points, fascial densifications, and faulty movement patterns/habits as contributing to many neuro-musculo-skeletal dysfunctions. This is logical and believable when one considers the expansive network of muscle and fascia (connective tissue) throughout the body, and how tissue overload and trauma can lead to dysfunction. The symptoms of many of these disorders are similar to those associated with RLS. While at this time there are no studies proving a correlation, one must consider that there is no more evidence supporting iron deficiency as the primary cause of RLS.
How is RLS treated?
As discussed earlier, simple blood testing may identify iron deficiencies which should be addressed. More commonly, RLS is treated with medication as noted above.3 While these medications function to diminish the symptoms of RLS, they do not resolve any underlying cause. This necessitates long-term use, which can be expensive, and in 40% of users medications can cause undesirable side effects such as drowsiness, dizziness, and nausea. Other more severe symptoms can occur including cardiac arrest, delirium, and aneurysm although these are less common.
Currently there is very little research concerning the effectiveness of exercise on RLS. A small study that compared exercise (resistance and aerobic) to no intervention showed improvement in symptoms at 6 weeks and this improvement was maintained through 3 months (the length of the study).3 There has also been very limited research conducted to investigate the effectiveness of soft tissue techniques (massage, myofascial release) on symptoms, although case studies have shown promising results.4
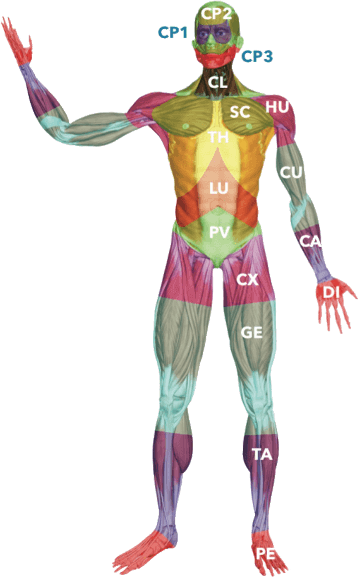
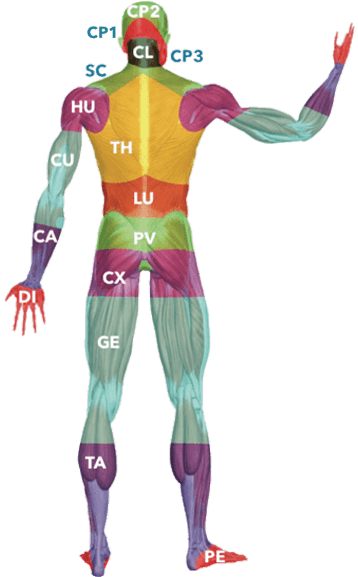
It has been our clinical experience that addressing myofascial trigger points in muscles, densifications in fascia, and faulty movement patterns that overload soft tissues in the trunk and extremities can help to diminish/resolve the symptoms of RLS. Our evaluation emphasizing movement assessment and palpation typically exposes soft tissue movement restrictions and biomechanical movement dysfunctions in the legs and other areas of the body.5 Very often, patients suffering with RLS demonstrate fascial restrictions in the feet and pelvic regions, which makes sense if you consider that the legs are then caught in the middle of a connective tissue tug of war. Often (although not always) RLS patients have a history of dysfunction involving the feet such as heel pain/spurs, plantar fasciitis, and bunions. Some relate a history dating back to childhood, often sadly diagnosed as “growing pains.”
Effective interventions we often utilize include a combination of dry needling, Fascial Manipulation®, and exercise including Postural Restoration® techniques. These approaches are utilized wherever needed throughout the trunk and extremities, as a global total-body approach is typically most successful. Home exercises are essential for addressing strength and movement issues that cause overload and dysfunction to the soft tissues. Education as to faulty habits and postures perpetuating problems is also essential to resolving the symptoms.
Many people are unaware of the options available to them in the management and resolution of RLS. We hope that this information has been helpful for you, and strongly encourage anyone suffering with RLS to explore these options. For further information or to speak with one of our therapists please contact our office.
References
- Ekbom, K., & Ulfberg, J. (2009). Restless legs syndrome. Journal of internal medicine, 266(5), 419-431.
- Chaudhuri, K. R., Appiah-Kubi, L. S., & Trenkwalder, C. (2001). Restless legs syndrome. Journal of Neurology, Neurosurgery & Psychiatry, 71(2), 143-146.
- Aukerman, M. M., Aukerman, D., Bayard, M., Tudiver, F., Thorp, L., & Bailey, B. (2006). Exercise and restless legs syndrome: a randomized controlled trial. The Journal of the American Board of Family Medicine, 19(5), 487-493.
- Russell, M. (2007). Massage therapy and restless legs syndrome. Journal of Bodywork and Movement Therapies, 11(2), 146-150.
- Day, J. A., Copetti, L., & Rucli, G. (2012). From clinical experience to a model for the human fascial system. Journal of bodywork and movement therapies, 16(3), 372-380.
Lymphedema is a swelling that typically occurs in the upper or lower extremities, due to an excessive buildup of lymph fluid. Your lymphatic system is part of your circulatory system, and it is a network of vessels that carry lymph fluid towards the heart. The lymphatic system is an essential part of your immune and circulatory systems.
When a blockage happens in your lymphatic system, swelling of your arms or legs may occur, as the fluid is not able to drain properly. Improper drainage results in a build-up of the lymph fluid in your arms and legs, which can generate adverse health risks. If you are suffering from lymphedema, contact Appalachian Physical Therapy today to find relief!
How do I know if I have lymphedema?
There are two categories of lymphedema: primary lymphedema, meaning it occurs on its own, and secondary lymphedema, meaning it occurs as a result of an alternative disease or condition.
Lymphedema typically occurs as a result of surgical treatment involving the lymph nodes. It is most common in surgical cancer treatments where the lymph nodes are removed or damaged. However, the cause of primary lymphedema isn’t always clear, and your physician may want to take additional imaging tests in order to look at your lymphatic system. This may include an MRI scan, CT scan, Doppler ultrasound, or lymphoscintigraphy.
The most common causes of secondary lymphedema include:
- Surgery
- Cancer
- Radiation treatment for cancer
- Infection
There are also a handful of symptoms that accompany lymphedema that could serve as indicators that you may have developed this condition. Keep in mind that it can sometimes take months or even years for lymphedema to develop as a result of cancer treatment.
Symptoms typically occur in the arms and legs, and they range from mild (noticing subtle changes or feelings in your limbs) to severe (noticing extreme changes or feelings in your limbs, to the point where they may be difficult to use).
Some common symptoms to look out for include, but are not limited to:
- Swelling
- Aching/discomfort
- Restricted range of motion
- Heaviness/tightness
- Infections
- Fibrosis
How is lymphedema treated?
With chronic swelling, there are many risks, including circulation issues, the risk of infection, and potential for future injury. It is very important to receive treatment for lymphedema and to follow up with your doctor and physical therapist on a routine basis.
At Appalachian Physical Therapy, we will design a personalized treatment plan to treat your lymphedema. This plan will be dependent upon your physical evaluation, health history, and the severity of your symptoms. For lymphatic treatment plans, the focus will be put strongly on manual therapy and light exercises.
A special type of manual therapy referred to as “manual lymph drainage” is commonly used for patients with lymphedema. It encourages the flow of lymph fluid in your upper and lower extremities, and additional massages may be used to increase circulation and provide relief.
Exercising the affected limb(s) also encourages lymph fluid drainage. Your exercise plan will be designed by one of our Harrisonburg, Broadway, and Pinehurst physical therapists and will involve gentle contractions of the muscles to regain function and improve your range of motion.
Additional treatments, such as wrapping, compression, or complete decongestive therapy may also be added to your treatment plan as our physical therapist deems fit. Contact our Harrisonburg, Broadway, and Pinehurst physical therapy office today if you are dealing with lymphedema and need some relief. Appalachian Physical Therapy will help reduce your lymphedema symptoms and improve your daily life. Your pain-free movement starts here!
What is Achilles Tendonitis?
Achilles tendonitis is an inflammation of the Achilles tendon that attaches your calf muscle to the back of your heel. Achilles tendonitis is typically caused by tightness in the hamstrings and calf muscles. In addition, limitations in ankle and foot range of motion can alter your walking pattern, putting excessive strain on the Achilles tendon, causing tendonitis.
Typically, the back of the ankle and heel is very painful to touch, especially after prolonged walking. Rest tends to help Achilles tendonitis while walking aggravates it.
How physical therapy helps
Physical therapy is one of the best treatment options for Achilles tendonitis. Our physical therapists will evaluate your leg, ankle and foot mobility, range of motion, strength, balance and walking patterns. This will help us discover the root cause of your pain and resolve that for long term results.
We focus on treatments to resolve your pain quickly, improve your joint mobility and strengthen muscles as needed. The result is the ability to walk and run without pain in the back of your heel returning to the activities you love to do.